In the Oklahoma Panhandle, where I grew up, if you keep your eyes peeled for the road-killed and the road-living, you soon begin to notice patterns: Tarantulas cross the road mostly in November, just before a freeze, or on misty 50-degree days in the spring. A hirsute kind of caterpillar tends to cross in early autumn, when it's still hot. Most of the animals I see on the road are in extreme circumstances— either dying to mate, like the box turtles I spot every summer, or simply dying. I find them fascinating even in their misfortune. We are bound to other animals by ties we hardly suspect— by the highways that link our cities and incise their habitats, by seasonal desires, even by the tiny parasitic lives hidden inside us all.
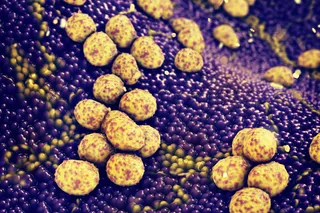
Armadillos not only carry leprosy, but They also have been expanding their range in america for more than a ...