He was dead. His face a terrifying, sweat-slicked white, the young man’s body lolled lifelessly on the emergency room gurney.
Five hours earlier, Marty had walked in a strong, healthy 27-year-old. His only worry: some sharp pains in the left side of his chest that started two days earlier. He figured it might be a muscle pull from weightlifting. But then it spread.
“Any shortness of breath?” I asked.
“No.”
“Pain down your arm?”
“Just the chest.”
“Do you smoke?”
“Half a pack.”
“Cough? Fever lately?”
“No, doctor.”
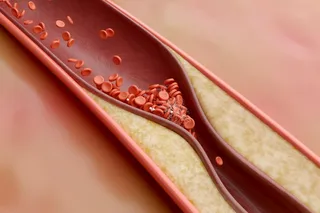
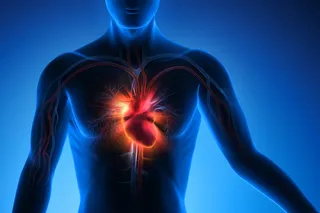
Marty was young for heart disease, but he was a smoker, I reminded myself.
“OK. Let’s take a listen.” With his shirt off, Marty’s compact frame bulged. On the left side, the sound of his breathing came through only faintly. Too much muscle? I wondered. But the right side sounded normal.
I stopped and asked, “You sure, no shortness of breath?”
“No, ...