In a packed emergency room, it's always a relief to see a straightforward case: 32-year-old male, light-headed, short of breath, vital signs normal.
Stressed young go-getters from Wall Street are common in this ER. Some days it seems every other patient arrives with palpitations, dizziness, chest tightness, tingling hands, and shortness of breath. All it usually takes is an electrocardiogram, some sincere reassurance, and they're on their way.
"Mr. Murphy," I said, entering the cubicle, "what can I do for you?"
"Don't know, doctor. Yesterday I was in line for theater tickets. It was very sunny and I hadn't had much breakfast. Next thing, I'm flat on my back."
"You passed out? Were you hyperventilating? Standing a long time?"
"Not really," he replied. "Then today I was still feeling dizzy and kind of out of breath when I got up."
"What do you do for a living?" I asked.
"I'm an accountant."
"No exposure to fumes, smokers, anything like that?"
"Nothing. I don't usually pass out."
I checked him from head to toe: utterly normal. No drugs, no excessive alcohol, happily married, healthy all his life. I had no reason to suspect any problem at all except perhaps a little tax-time stress.
"Everything seems fine," I told him confidently. "We see a lot of this. I'll get your discharge papers."
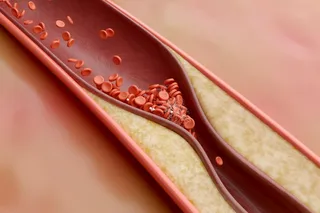
On my way out I glanced at the pulse oximeter: 96. This instrument measures oxygen levels in the blood. A normal reading, especially in a healthy young man, should fall in the high 90s. I stopped and watched. It drifted down to 92.
"You know," I said, trying to sound casual, "this machine says your oxygen level may be a tad low. We should verify it with a blood gas test. Hurts a bit, because I'll have to take blood from your wrist artery."
"Sure," he replied, sounding relieved, "you check everything you need."
The blood gas confirmed that his oxygen level was two thirds what it should have been. A chest X ray explained why: Around the center of Mr. Murphy's chest sprouted potato-sized lymph nodes. Sarcoidosis. And I had almost sent him home.
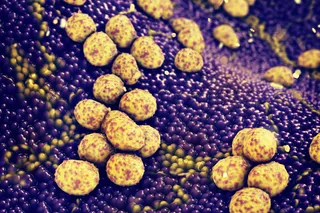
The very name, just latinizing the obvious, hints at how little we know about the disease. "Sarco" means flesh; "sarcoidosis" equals fleshy growths all over the place. First described 120 years ago in a patient with purplish skin lesions and kidney failure, it has an underlying cause as mysterious now as it was then. The hallmark is granulomas: immune cells that cluster as they do when lymph nodes react to a local skin infection, tonsillitis, or mononucleosis. In sarcoidosis, however, the inciting villain remains unknown. We do know, however, that for some reason macrophages (scavenger cells) and lymphocytes (the immune fighters trained to remember pathogens) start secreting proteins that spark an immune-cell population explosion.
Sarcoidosis is a disease with a dozen faces. It most commonly affects the lungs. Doctors often first detect the disease when a routine chest X ray turns up enlarged lymph nodes in an otherwise healthy young person. In many cases, though, the first sign is shortness of breath. But sarcoidosis can also show up as a bout of fever, malaise, weight loss, or as a profusion of skin lumps and joint pains. Sometimes patients suffer eye inflammation, cheek swelling, and facial nerve palsy. In more worrisome cases, the granulomas can sprout in heart or brain tissue.
Most intriguing is a connection with tuberculosis. The knots of cells in sarcoidosis bear a resemblance to the lesions of tuberculosis. But when sarcoidosis patients are challenged with a skin test that evokes immune responses to tuberculosis, they tend to react less dramatically than would be expected if sarcoidosis were caused by a TB kin. A possible, paradoxical reason may be that a dramatic overreaction to the TB bacillus or its benign cousins produces the clusters of immune cells; perhaps the skin test is simply too trifling a stimulus for an immune system already coping with a TB-like infection elsewhere. But efforts to find DNA evidence of the TB bacterium in sarcoidosis lesions haven't proved the connection.
The devilish thing about sarcoidosis is its unpredictability. In most parts of the world, at least half of new cases clear up spontaneously. On the other hand, many of the rest incur some form of permanent lung abnormality, and one in 10 cases shows a progressive scarring of lung tissue.
"Mr. Murphy," I began, "you have a disease called sarcoidosis. It's basically an immune-system overreaction. In some cases we just watch and wait. But given how short of breath you feel, the pulmonologist may decide to treat you with steroids to help shut down the immune response. The good news is, they are usually very effective."
"How did I get this?" he asked.
"No one knows what causes sarcoidosis," I replied. "What we know is that it tends to strike some groups more often than others, but we don't know why. In the United States, for example, African-American women are about 15 times more likely to develop it than white males. In London, however, the disease is endemic among Irishwomen who have emigrated there."
"Last I heard, my mom was Swedish," he said. "Dad's of German extraction. Not sure where the Murphy snuck in."
The pulmonologist, eyeing the chest X ray, declared the case "classic" but said Mr. Murphy would still need a biopsy: "Lymphoma and some fungal infections can fool you."
"Steroids?" I asked.
"We'll watch him for a few months, see whether it progresses. These incidental pickups . . . "
"But his blood gas was only 59, and he passed out yesterday."
"Right," he said, lightly smacking his forehead. "I knew that."
The fainting episode, a potential harbinger of heart trouble, was the first symptom to study. Cardiac sarcoidosis can sometimes lead to sudden death in young people. On the other hand, our patient had been standing in the sun for a while, the oxygen level in his blood was already low, and he'd had little breakfast— three good reasons to faint. The electrical activity and structure of his heart— as measured by an electrocardiogram and an echocardiogram— were normal, so cardiac sarcoidosis seemed unlikely.
The following day, the pulmonologist examined Mr. Murphy's windpipe through a fiber-optic bronchoscope. It looked somewhat narrowed, probably from the lymph nodes bunched around it, but nothing serious. With a tiny forceps, he poked through the cartilage to sample surrounding lung tissue.
Two days later, the pathology report came back: sarcoid. Lymphocytes had not only packed themselves into the chest lymph nodes but also spread throughout the delicate alveoli, the membranes where gas exchange occurs in the lungs. That explained the difficulty breathing.
"He's decided to go for the steroids," the pulmonologist said. "Even more advanced cases can remit on their own, but why wait for worse?"
Steroids are no free lunch. Their side effects can include weight gain, osteoporosis, and diabetes. And while steroids suppress sarcoidosis, they do not cure it. Treated and untreated patients, 10 years after diagnosis, seem to have the same rates of disease progression or complete remission. On the other hand, steroids can make patients feel better, even if the outcome remains the same.
Three months later, the pulmonologist gave me an update.
"The chest cleared like that," he said, snapping his fingers. "And we've got the steroids down to almost nothing. He feels great. But keep your fingers crossed. With sarcoid, you never know."