When I met Judy, I had just finished seeing what seemed like 100 diabetic patients, one after the other. As an endocrinologist, I specialize in the management of hormonal disorders, and this is business as usual for me: More than 60 percent of my patient visits focus on diabetes.
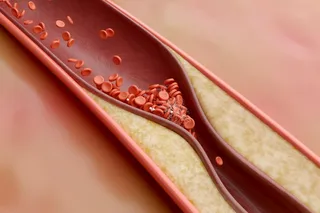
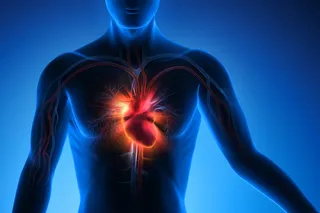
I picked up my last chart of the morning and saw that it was another new patient with Type 2 diabetes. Judy was 47 years old, and as a result of her illness, she already had suffered several heart attacks and developed eye and kidney damage. She also had blockages in the major arteries that supply her legs with blood, and she had dangerously high blood pressure. I flipped through Judy’s chart, noting no other unusual medical problems. Although she clearly had severely uncontrolled diabetes, the case seemed pretty routine.
Then I entered the room — and saw something far from ...