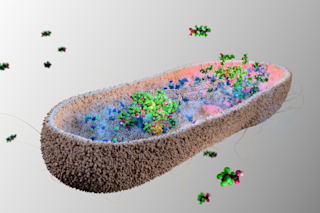
Microbiome: Your Body Houses 10x More Bacteria Than Cells
Explore our stunning image gallery showcasing beautiful visuals, perfect for lazy loading images to enhance your site.
More on Discover
Stay Curious
SubscribeTo The Magazine
Save up to 40% off the cover price when you subscribe to Discover magazine.
Subscribe